
The presence of an SVP viewed upon direct ophthalmoscopy may suggest that an elevated disc is not secondary to increased intracranial pressure.Additionally, no RNFL thickness value reliably differentiates papilledema from pseudopapilledema. With OCT, the optic disc drusen appear as hyporeflective structures with a hyper-reflective margin. The ODDS Consortium recommends the use of enhanced-depth OCT imaging for adequate visualization of disc drusen. As technology improves, OCT is increasingly used in the diagnosis of optic disc drusen.

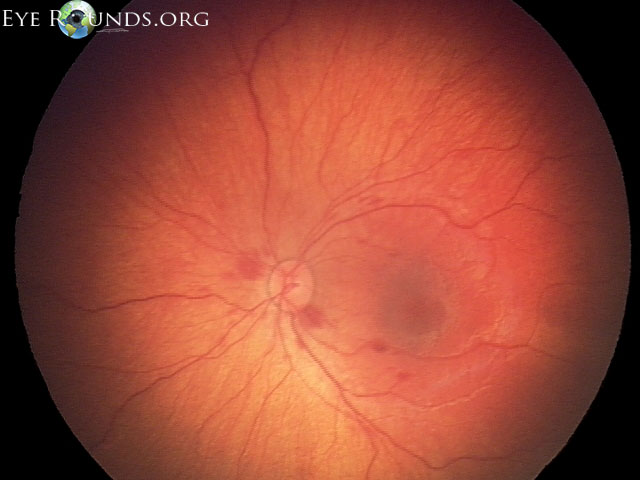
B-scan remains the standard for assessing presence of buried optic nerve head drusen.However, patients with optic disc drusen may also have overlying edema, and the buried disc drusen will not hyper-autofluoresce. Fundus autofluorescence may help to highlight optic disc drusen, which appear hyper-autofluorescent.OCT of the peripapillary RNFL can be particularly helpful, as the en face images can reveal subtle peripapillary wrinkles that would otherwise be difficult to view funduscopically.Papilledema is, by definition, optic disc edema in the setting of increased intracranial pressure and is a medical emergency. Causes of pseudopapilledema are relatively benign and include buried optic disc drusen and small, anomalous and/or hypoplastic discs. Pseudopapilledemaĭifferentiating these clinical entities can be quite challenging. 1 Imaging showed no evidence of intracranial mass or venous sinus thrombosis however, she did exhibit low-lying cerebellar tonsils concerning for Chiari I malformation. MRI is the preferred neuroimaging modality due to superior soft tissue resolution and better visualization of particular findings consistent with intracranial hypertension such as optic nerve sheath distension, empty sella and posterior globe flattening. In addition, upon analysis of the vitreoretinal interface on optical coherence tomography (OCT), she demonstrated subtle peripapillary wrinkles in the left eye, suggestive of mild papilledema ( Figure 2).ĭue to her ocular findings, she was sent for urgent neuroimaging that included magnetic resonance imaging (MRI) of the brain and magnetic resonance venography of the head to rule out a mass and venous sinus thrombosis. She exhibited no spontaneous venous pulse (SVP). She denied any other symptoms or use of tetracyclines, vitamin A derivatives or oral contraceptives. When asked about symptoms of increased intracranial pressure-such as headaches, pulsatile tinnitus, nausea, vomiting, diplopia and transient visual obscurations-the patient reported occasional headaches and “seeing stars” when she bent down. The optic disc photos demonstrate elevation OS>OD, raising the question of papilledema vs.

In this patient’s en face OCT vitreoretinal interface image of the left eye, note the wrinkles superior temporal, consistent with Paton’s lines or peripapillary wrinkles that are not readily visible funduscopically. Her dilated fundus exam revealed subtle elevation more so in the left eye than the right ( Figure 1).įig. She was above her ideal body weight at 240lbs. Her blood pressure was elevated at 142/86mm Hg RAS. Intraocular pressures (IOPs) measured 16mm Hg OD and 15mm Hg OS. Her anterior segment exam was remarkable for palpebral conjunctival pallor, consistent with her history of anemia. She exhibited 90% of normal abduction bilaterally with no diplopia and a 2 to 4 prism diopter comitant esophoria in all gazes.
#Od and os which is right and left full#
Entrance testing was unremarkable with 20/20 vision uncorrected OD and OS, full confrontation visual fields bilaterally and no relative afferent pupillary defect. Her health history was remarkable for hypothyroidism, asthma and iron-deficiency anemia. Click image to enlarge.Ī 43-year-old African American female presented for her annual exam without any visual complaints. Despite unremarkable entrance testing with no visual complaints, the patient’s optic disc evaluation shows mild elevation with sectoral blurred margins nasally and superiorly OU. This case-based review provides photos and clinical pearls to help you enhance your assessment of optic disc abnormalities.įig. Clinicians must take a systematic approach to optic disc evaluation, carefully assessing the margins, color of the neuroretinal rim, cup-to-disc ratio and overall size of the nerve. When a disc is not “perfused, healthy, distinct and flat,” it can be difficult to differentiate between anatomic variations and pathology. Accurate evaluation of the optic disc is a critical part of optometric practice.


 0 kommentar(er)
0 kommentar(er)
